If you’re looking to outsource your urology medical billing services, chances are you’re coming across a lot of different billing companies, all claiming to offer the best solutions. This can leave urology practices struggling to choose a company that focuses on their needs and can handle the complex issues specific to their office.
Once you finish this short blog, you’ll understand urology medical billing well, including what these services include, how they target specific complexities, and the most common mistakes coders and urologists experience.
What Is Urology?
Urology focuses on diagnosing and treating various conditions affecting both male and female urinary organs, including the kidneys, bladder, ureters, and urethra, as well as the male reproductive organs, such as the prostate, testes, and penis. Without urologists, individuals can experience severe health problems, including cancers, urinary tract infections, kidney stones, prostate disorders, incontinence, and difficulties with sexual function.
Urologists usually collaborate with other medical specialists, such as nephrologists (kidney specialists), oncologists (cancer specialists), and gynecologists (female reproductive system specialists), to provide comprehensive care for patients with complex urological conditions.
Most urology surgical procedures are minimally invasive or can be effectively treated on an outpatient basis (ambulatory surgery), allowing patients to return home on the same day as their surgery. This is where ASC medical billing services come in.
How Do Urology Medical Billing Services Work?
Urology procedures can be complex and costly, making accurate medical coding and billing crucial for healthcare providers to receive reimbursement on time and for the right services. Due to this, many providers outsource their urology medical billing to specialized companies to focus on their patients and streamline the process. Otherwise, urologists and their staff can get caught up with coding, billing, and following up on claims and denials.
If you’re looking for a medical billing company specializing in urology, here’s everything you should look for and check off before making calls.
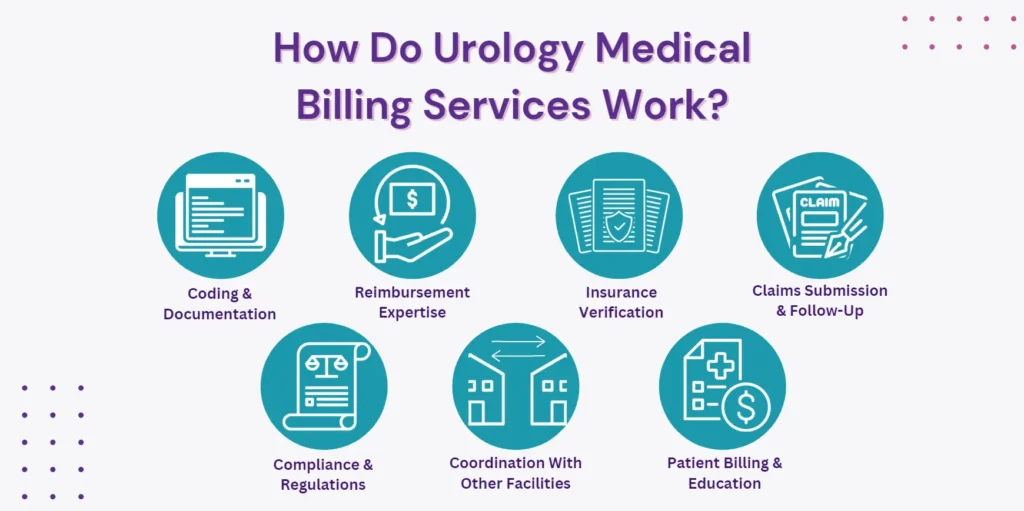
- Coding and documentation: Look for a professional billing company well-versed in the specific medical codes used in urology. They should ensure accurate identification and billing of procedures and services to insurance companies or third-party payers.
- Reimbursement expertise: The billing company should have a thorough understanding of reimbursement processes and regulations related to ambulatory surgery medical billing, including coding systems, insurance policies, and practice guidelines.
- Insurance verification: Ensure the billing company verifies patient insurance coverage and obtains necessary authorization before you provide services. This helps prevent claim denials or payment issues. The verification process should cover confirming benefits, co-pays, deductibles, and pre-authorization requirements.
- Claims submission and follow-up: The chosen billing company should ensure accurate claim submission with necessary supporting documentation. Additionally, they should monitor claim status, follow up on denials or rejections, and promptly address any issues or discrepancies.
- Compliance and regulations: Look for a billing company that adheres to various compliance regulations, including HIPAA and insurance company guidelines. Compliance ensures patient privacy protection and accurate billing practices.
- Coordination with other facilities: If your urology services involve coordination with other surgery centers or hospital facilities, ensure the billing company can handle the billing aspects related to separate components like facility fees and anesthesia services.
- Patient billing and education: Billing companies should effectively address patient billing concerns and clearly explain costs and insurance coverage to patients and practices.
Key Things To Look For In Urology Billing Services
While many outsourced companies provide standard billing solutions, it’s better to seek a company surpassing conventional billing and coding services.
- Pre-Payment Review (PPR) and Provider Network Integrity (PNI) audits: A reliable billing service should guide you through routine PPR and PNI audits, helping your staff ensure compliance and minimize errors.
- Advocacy: Look for a billing service that can help you address issues with payers and engage in corrective actions to restore relationships.
- Data analysis: Their billing services should be able to create benchmarks for your practice and compare them to industry norms and trends, helping you identify areas for improvement.
- Education: Seek a billing service that can provide guidance and support in navigating the complexities of regulatory environments.
- Denials management: If you face denied or underpaid claims, a comprehensive billing service with legal expertise can escalate the issue on your behalf.
- Business decisions: Look for a company offering insights specific to your geographical area, helping you make informed decisions to grow your business strategically.
- Negotiations: A reliable billing service should assist you in pursuing in-network contracts or adding new service lines to expand your practice.
- Customer service: Seek a billing service that prioritizes customer service and can help you implement telehealth solutions to improve patient access and care.
Free eBook: The Benefits Of Outsourcing Your Medical Billing
Why Is Urology Medical Billing Complex?
Urology medical billing involves several specific complexities due to the unique nature of procedures and overlap with other specialties such as oncology, gastroenterology, andrology, pediatrics, endocrinology, and gynecology. Some of the specific complexities include:
- Procedure coding: Urologists perform a wide range of procedures, such as cystoscopies, lithotripsies, nephrectomies, and ureteroscopies, each with its own specific codes that need to be properly identified and billed. Each insurance company may have specific rules regarding coverage and reimbursement rates for different urology services.
- Diagnosis coding: Urologists diagnose and treat conditions such as urinary tract infections, kidney stones, prostate disorders, and bladder cancer. Correctly documenting and coding the diagnoses is crucial for accurate billing and reimbursement.
- Surgical billing: Urologists often perform both minimally invasive and open surgical procedures. In some cases, these procedures involved other facilities and fees. For instance, accurately coordinating the billing for a robotic-assisted laparoscopic prostatectomy would require separate coding for the surgical procedure, facility fees, and anesthesia services.
Common Mistakes Made During In-House Urology Medical Billing
Most urology practices miss out on about 10-20% (approximately) of their reimbursements because of inefficient processes, lack of skilled staff, inexperience, inadequate use of technology, and ineffective management.
- Inaccurate patient information: Failing to obtain correct patient demographics, insurance information, social security number, and valid address can lead to billing errors and claim denials.
- Errors in healthcare centers’ information: Neglecting to verify your healthcare center/practice’s correct name, address, contact numbers, identification numbers, and EDI processing numbers can result in billing inaccuracies.
- Insufficient review of denied claims: Resubmitting denied claims without thorough review can lead to repeated rejections. It is important to carefully examine the reasons for denial, such as missing or incorrect coding, and consult with a urologist to ensure accurate diagnosis codes are used.
- Double billing: Submitting duplicate claims for specific provisions of insurance payers, such as postoperative visits, can result in non-reimbursement or policy violations. Adhering to the guidelines and instructions provided by insurance payers, including Medicare, is essential to avoid double-billing.
Contact Hansei Ambulatory Surgery Billing Solutions
If you want a medical billing company that takes revenue cycle management to a new level, contact Hansei Ambulatory Surgery Billing Solutions. Hansei Solutions recognizes the distinct challenges encountered by ASCs and provides comprehensive medical billing services that extend beyond mere claims processing and collections. Call today to book a demo and learn more about how Hansei can grow your business from a small practice to a leading healthcare facility.