Credentialing in medical billing helps healthcare practices verify their physician’s qualifications and expand their in-network accepted insurance plans to increase patient growth and satisfaction. If this process is done incorrectly or not at all, healthcare providers can quickly lose revenue and patients if their physicians and nurses are waiting for insurance companies to approve them, unable to provide essential services.
This article explains how credentialing in medical billing works, why it’s important, the most common challenges faced during the credentialing process, and the benefits of efficiently outsourced medical credentialing.
How Does Credentialing In Medical Billing Work?
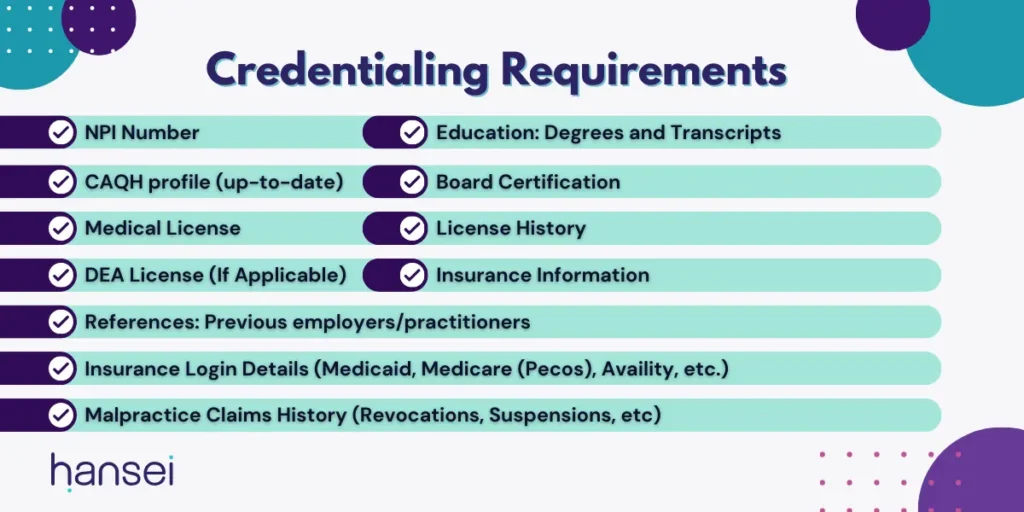
All healthcare providers, from registered nurses to occupational therapists, are required to have degrees, licenses, or certifications that qualify them to provide their specific services. Before each physician joins your team and starts providing healthcare, their credentials must be submitted and verified by internal credentialing departments, insurance providers, and government programs like Medicare and Medicaid.
This ensures they have the proper qualifications to provide care to patients since unlicensed medical care is a criminal offense in most states, and most patients want experienced professionals to diagnose and address their conditions. Previously, requesting and submitting provider credentials was time-consuming and could take over three months to complete. If a practice was onboarding a physician or staff, it could have been months before they could physically see patients.
Types Of Credentialing Services
- Individual Provider Enrollment: Individual provider enrollment is the process of verifying the qualifications and credentials of an individual healthcare provider (such as a physician, nurse practitioner, or dentist) to ensure they meet the standards required by healthcare organizations or insurance networks.
- Group Provider Enrollment: Group provider enrollment refers to enrolling an entire medical group, clinic, or practice with a healthcare facility, insurance company, or other payer.
- Primary Source Verification: Primary source verification involves directly contacting the original source of a credential (such as a medical school, licensing board, or certification organization) to independently verify the accuracy of the information provided by the healthcare professional.
- Recredentialing: Recredentialing is the process of periodically verifying the credentials of healthcare providers at regular intervals to ensure continued quality and safety of patient care.
- Credentialing Appeals: If a provider’s application is denied or privileges are restricted, they can appeal the decision and provide additional information to support their case.
Credentialing Organizations
- Council for Affordable Quality Healthcare (CAQH): CAQH is a nonprofit organization that offers a platform for providers to submit and maintain their credentialing information electronically. It streamlines credentialing by allowing providers to share their information with their insurance board members, including Aetna, BlueCross Blue Shield, United, and Humana.
- National Committee for Quality Assurance (NCQA): NCQA is a nonprofit organization that accredits and certifies healthcare organizations, including health plans and medical practices. It sets standards for quality care and patient safety, and its accreditation indicates that an organization meets specific quality criteria.
- The Joint Commission (TJC): The Joint Commission is an independent nonprofit organization that accredits and certifies healthcare organizations and programs in the United States. It focuses on evaluating and improving patient safety and the quality of healthcare services provided by hospitals and other healthcare facilities.
The Most Common Credentialing Challenges
Some of the most common credentialing challenges faced by healthcare providers and underequipped medical billing companies include:
- Your practice is falling behind: Credentialing, which involves verifying a lot of data, can be a slow and tedious process. Depending on how complicated healthcare services are, it might take around 3 to 4 months, or even longer, and sometimes more information could be required. If healthcare services stretch across different countries and need to follow diverse healthcare laws, the requirements for credentialing would also change accordingly.
- Sudden medical changes: Even simple things like updating surgical tools, adopting new medical technologies, or shifts in a medical professional’s skills can trigger the need for recredentialing. Since all these services are closely linked, the credentialing process can become intricate.
- Application mistakes: A major error that healthcare providers can make is leaving out, misrepresenting, or accidentally entering the wrong details in their applications. Since the application is crucial for credentialing, mistakes can lead to outright rejection. This rejection could have lasting consequences. Insurers might refuse to work with the provider in the future, and if they agree to work together later, it will come with strict conditions.
- Unaware of requirements: Medical credentialing rules differ from state to state. For example, 28 states follow a reciprocity law, which allows healthcare providers to practice in multiple states without needing to get a new license or undergo more education. However, states with reciprocity laws have their own specific requirements for credentialing.
- Poor onboarding process: Before a medical practitioner starts practicing, they usually undergo a preliminary assessment at a medical facility. Then the facility arranges an agreement or contract with an insurance company, enabling the practitioner to treat patients. But the medical facility needs complete and accurate information about the practitioner they are trying to credential. Not having enough information about the candidate can cost your medical practice cash flow, patients, and the ability to provide healthcare.
Read more: Top 3 Medical Billing Mistakes That Lead To Claim Denials
An Efficient Credentialing Process Improves Reputation
Credentialing in medical billing doesn’t just improve how quickly you can bill insurance for providing healthcare. Providers like dentists, orthopedics, dermatologists, and others rely on reputation as much as they rely on quality care.
- Patients will be more confident in your practice: When patients trust their doctors and nurses, they’re more likely to follow through with treatment plans, make changes to their diet or routine, and return to your practice. You can’t have an unlicensed medical staff, and patients won’t trust your practice if no one is qualified to assess their medical conditions.
- Physicians looking for work will trust your practice: An efficient and speedy credentialing process will display to physicians who are looking to join a practice that your office is professional. If they witness your ability to onboard and credential staff, they’ll know your intention to keep them and contribute to their professional experience.
- Other practices will be confident you can handle referrals: Many medical practices refer their patients to other specialties if they realize the need for another expert. Dentists can refer patients to orthodontists who want braces or aligners, while ears, nose, and throat doctors can refer a client to a gastroenterologist if their issues have spread to their stomach.
- Your payors will trust your practice: Insurance providers require healthcare providers to verify their physician’s credentials before they accept medical bills or refer clients to their practice. Once a payor is familiar and confident with your practice’s skills, they can be more susceptible to renegotiating managed care contracts.
Read more: Healthcare Patient Retention: Importance, Strategies, & Calculation
Contact Hansei Solutions For Medical Credentialing
If your medical practice is struggling with its credentialing and medical billing process, contact Hansei Solutions. Our medical credentialing team can help you onboard physicians and healthcare staff quickly, so you can start providing essential medical services, improve relationships with insurance plans, and boost your patient’s confidence in your expertise and professionalism. Call today, and one of our credentialing experts can answer any questions, tell you about our onboarding process, and set you up with a demo of our services.


